 (WTTW News via CNN)
(WTTW News via CNN)
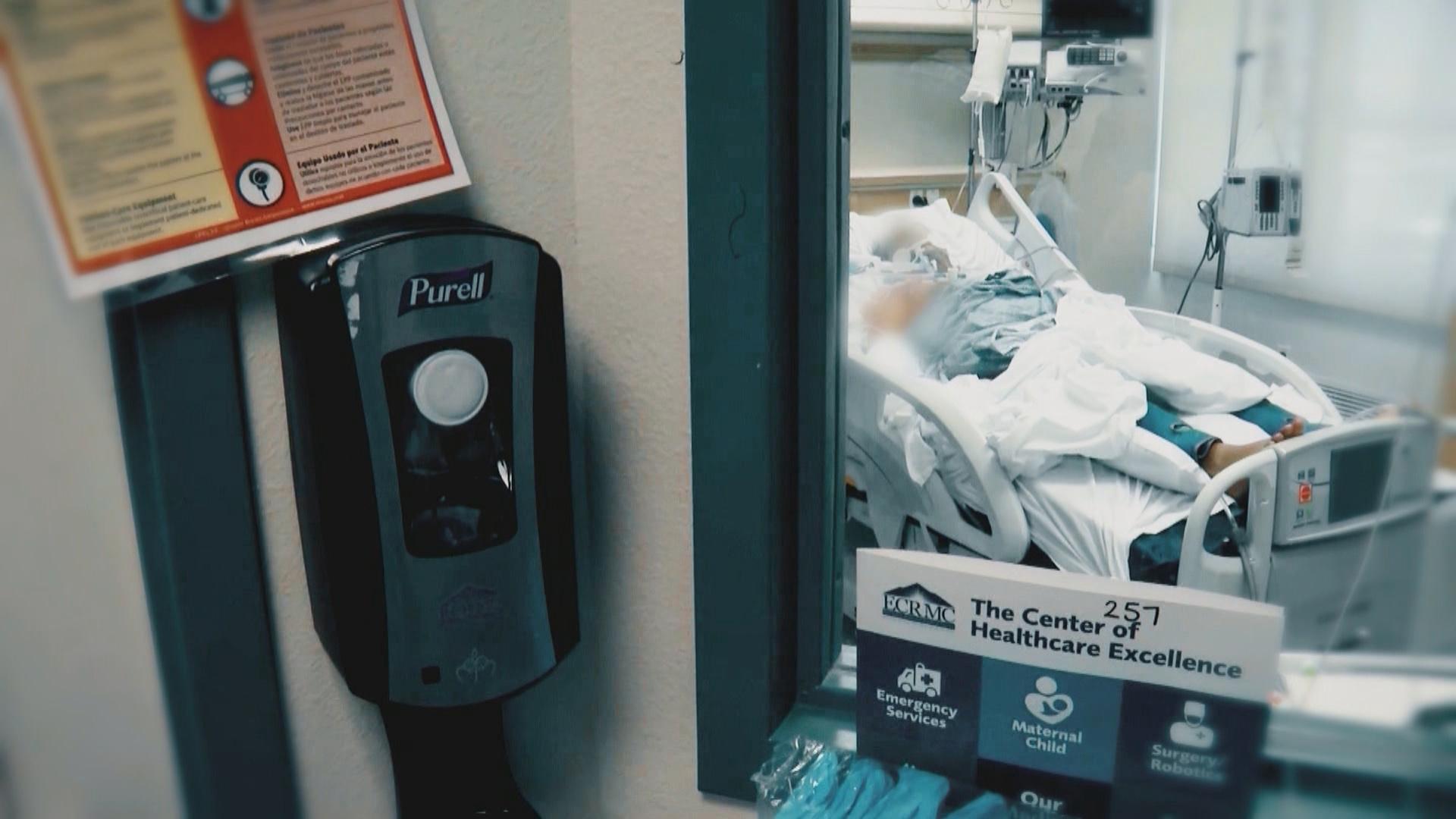
It’s no secret that Illinois is having major budget difficulties due partly to the COVID-19 pandemic.
Thanks to our sponsors:
The state pays billions of dollars into the Medicaid program that covers more than 2 million residents. WTTW News has learned that a group of lawmakers plans to demand billions of dollars back from the private health care organizations that run Illinois’ Medicaid program.
State Sen. Dave Koehler (D-Peoria) and state Rep. Fred Crespo (D-Streamwood) say they believe it’s time for private health insurance companies that have seen big profits since the pandemic began to make sacrifices.
Illinois paid more than $16 billion to managed care organizations in fiscal year 2020 to administer the state’s Medicaid program. Roughly half of state Medicaid payments are reimbursed by federal tax dollars.
Crespo and Koehler say they plan to file a bill Wednesday in the General Assembly that would, in effect, give the state the ability to wrest back 20% of that money should the governor issue a disaster declaration, as he did on March 9, because of COVID-19.
The bill also calls for those savings to be redirected to fund critical care and safety net hospitals throughout the state, many of which are under-resourced and, in the case of Mercy Hospital on Chicago’s South Side, planning to close. Crespo says that the private insurance organizations that run Illinois’ Medicaid program can afford to give some of that money back.
“We know that hospitals have not been doing services they normally do, elective surgery,” Crespo said. “So costs have gone down. So the plan here is to say, we should take back 20% of (the managed care organizations’) profits and redirect it to other Medicaid expenses the state has.”
According to 2019 data from the Illinois Department of Healthcare and Family Services, there are six organizations that run the Medicaid Managed Care program in Illinois. The largest are Meridian Health, with 800,000 enrollees; Blue Cross Blue Shield, with 390,897; and County Care, which is run by the Cook County Health and Hospital System and enrolls 317,846 members. The state paid more than $16 billion to Managed Care Organizations in fiscal year 2020, and is on track for a similar payment this year, according to data from the Illinois Comptroller’s office. The payment is determined by a capitation rate, or a fixed amount the state agrees to pay per patient, per unit of delivery.
In the second quarter of 2020 alone, the parent company of Blue Cross Blue Shield saw profits of more than $2 billion, doubling its performance from the year prior.
Koehler says health insurance companies should follow the lead of other industries that have helped consumers out during the pandemic.
“Take the auto insurance industry, they’re giving rebates to their customers because people aren’t driving as much,” he said. “Even cable companies are saying, ‘We’re going to give you some of your money back.’ There are a lot of industries that have set the pattern for this to say, ‘Hey let’s help people out during a pandemic.’”
Even if the bill passes, there are questions as to whether the state can legally claw back money it is contractually obligated to pay. Industry representatives say the bill could have severe negative implications for the millions of Medicaid patients in Illinois, and that there are already provisions to return tax dollars if health care utilization rates go down.
“Should utilization drop back down again, and health care costs increase, there’s already a provision in the contract where the health plans would return dollars to the state they could use to invest in education or other funding sources,” said Samantha Olds Frey, CEO of the Illinois Association of Medicaid Health Plan. “We’re not currently seeing a decrease in utilization or costs anywhere near the level of 20%.”
The proposal is another attempt from some lawmakers to scrutinize Illinois’ controversial Managed Care System. The state has gradually transitioned out of a more traditional, state administered fee-for-service health care system over the last seven years. Former Illinois Govs. Pat Quinn and Bruce Rauner both moved the state to the current model, paying outside organizations lump sums to run Medicaid like traditional HMO plans.
A 2018 audit from the state inspector general found that Illinois was not keeping track of the billions of dollars the Managed Care Organizations paid in claims or what claims they denied. The state also did not keep track of the administrative costs paid to these organizations to manage the system.
Crespo says he’s long wanted the state to go back to what Medicaid used to be.
“It’s really a shame that we’re using a model that incentives profits at the expense of health care for those that need it the most,” Crespo said. “This goes contrary to any democratic principals and values that we have.”
Follow Paris Schutz on Twitter: @paschutz
Note: This story will be updated.
Thanks to our sponsors:
Thanks to our sponsors:
"back" - Google News
December 09, 2020 at 04:41AM
https://ift.tt/39VlFFk
Illinois Lawmakers to Demand Billions Back from Health Insurers Due to COVID-19 - WTTW News
"back" - Google News
https://ift.tt/2QNOfxc
Shoes Man Tutorial
Pos News Update
Meme Update
Korean Entertainment News
Japan News Update
Bagikan Berita Ini















0 Response to "Illinois Lawmakers to Demand Billions Back from Health Insurers Due to COVID-19 - WTTW News"
Post a Comment